Accurate diagnosis of neurodegenerative diseases is hindered by the inaccessibility of the brain and is mainly based on the evaluation of clinical features. However, overlapping symptoms across related disorders might confound diagnosis and delay proper intervention. Moreover, as clinical manifestation is preceded by an asymptomatic prodromal stage during which neuronal degeneration is ongoing, these disorders are often diagnosed at an advanced stage. The goal of my group is to develop a biomarker panel based on the quantification of DNA methylation of selected genes that can discriminate PD patients from healthy subjects in a simple blood test. This highly innovative approach represents the core of our translational research.
Leveraging our multiple studies in blood methylation, including cohorts from the National Institutes of Neurological Disorders and Stroke, the Harvard Biomarkers Study (HBS), and the Parkinson’s Progression Markers Initiative (PPMI), we are defining candidate biomarkers for disease progression and responses to medications.
We completed the first longitudinal study of blood methylation biomarkers in PD (Henderson-Smith et al. Epigenetics 2019); a collaborative endeavor with researchers at Arizona State University and the HBS which included ~ 800 samples and identified dynamic changes in blood methylation that accompany disease progression. This work uncovered a previously unsuspected effect of dopaminergic therapies on blood methylation.
We are currently performing methylomic analyses on a large cohort of the PPMI, a study funded by the Michael J. Fox Foundation, and including more than ~2,400 longitudinal blood samples from prodromal, idiopathic, and genetic PD patients in comparison to healthy control individuals.
DNA methylation markers to classify Lewy Body disorders
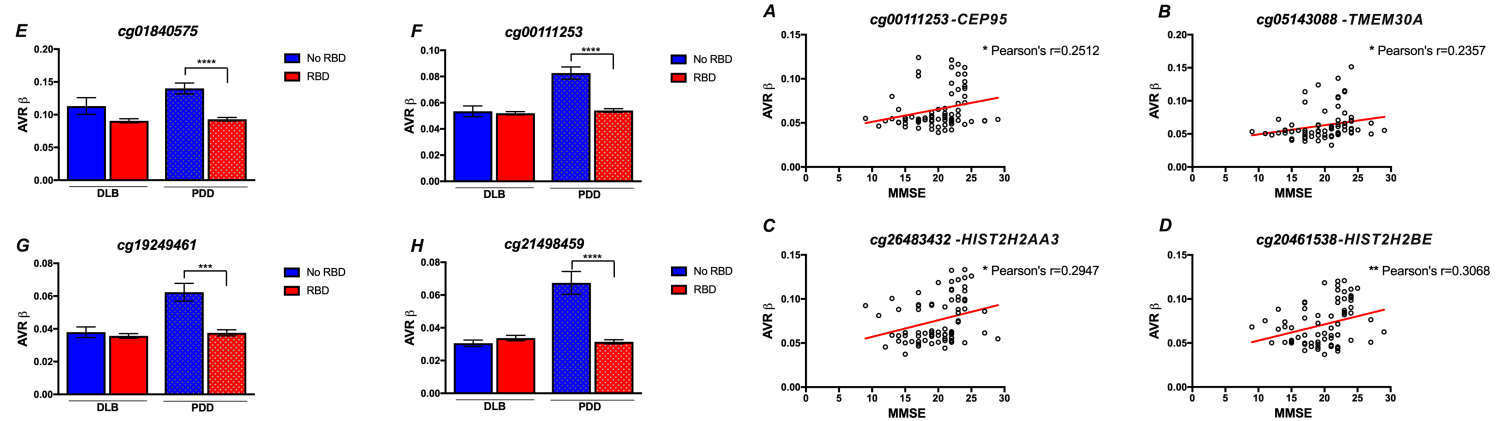
Lewy body diseases (LBD) are a heterogeneous group of disorders characterized by the accumulation of α-synuclein in Lewy body structures in the brain. LBD, including PD-Dementia (PDD) and Dementia with Lewy Bodies (DLB), present with a wide clinico-pathological variation, and differentiation between these disorders is based on the type and timing of clinical manifestations. However, the lack of specific biomarkers hampers determination of clinical subtypes in LBD. Expanding our work on PD biomarkers, we have also completed the profiling of blood methylation in DLB and PDD cases in collaboration with the Harvard Biomarker Study and Parkinson’s Disease Biomarkers Program. Our results uncovered unique methylation profiles that differentiate both disorders, revealing methylation sites associated with cardinal features of disease, including cognitive decline and REM-sleep behavioral disorder. Notably, we identified a set of differentially methylated sites that show promise as disease classifiers. Read the complete study at Nasamram et al. Alzheimers Dement (Amst). 2021 Feb 20;13(1):e12156.
